Advancing inclusive DR-TB treatment: reflections from the BDLLfxC global learning session by PeerLINC
As countries accelerate the shift toward shorter, all-oral regimens for drug-resistant tuberculosis (DR-TB), a new conversation is emerging around the groups who have long been left behind: children, pregnant people, and lactating women. PeerLINC’s recently concluded global webinar on BDLLfxC brought together program managers, clinicians, researchers, and implementing partners from across high-burden settings to reflect on how this regimen is expanding possibilities for more inclusive and equitable DR-TB care.
The BDLLfxC regimen (Bedaquiline + Delamanid + Linezolid + Levofloxacin + Clofazimine), now recognized in the latest World Health Organization (WHO) DR-TB guidelines, is building on previous advances in shortening TB treatment to bring the same benefits to an expanded population.
Filling long-standing gaps and reimagining what inclusive treatment means
In her presentation, Dr. Francesca Conradie, infectious diseases expert and principal investigator of the BEAT Tuberculosis (BEAT TB) trial in South Africa, reflected on the DR-TB treatment landscape before shorter regimens became a reality. For years, therapy was long, toxic, and devastating for many families. And even after the introduction of BPaLM/ BPaL, some remained excluded.
““We wanted to fill that gap for both pregnant women and children,” she explained. “It seemed unfair that a household exposed to the same strain of TB would receive entirely different regimens—six months for the father, but nine to eighteen months of difficult treatment for the mother and child.””
Her message resonated deeply because it speaks to a structural inequity that programs encounter every day. What BDLLfxC offers is clinical feasibility and dignity, by allowing entire families to access the same standard of care.
The evidence from South Africa’s BEAT TB trial, where BDLLfxC achieved 86% treatment success, opened the door to the WHO recommendation and to a broader realization that shorter, safer, and more tolerable treatment for maternal and pediatric patients is now possible.
Dr. Conradie also emphasized BDLLfxC’s practicality for programs needing to start treatment promptly. As she explained, “We wanted a regimen that we could begin almost immediately without having to wait for further susceptibility tests. Once the fluoroquinolone resistance result becomes available, the regimen can then be adjusted accordingly. If the patient turns out to be fluoroquinolone susceptible, we stop clofazimine; if resistant, we stop the levofloxacin.” This flexibility is vital in settings where drug-susceptibility testing (DST) delays can cost weeks—time that many patients cannot afford to lose.
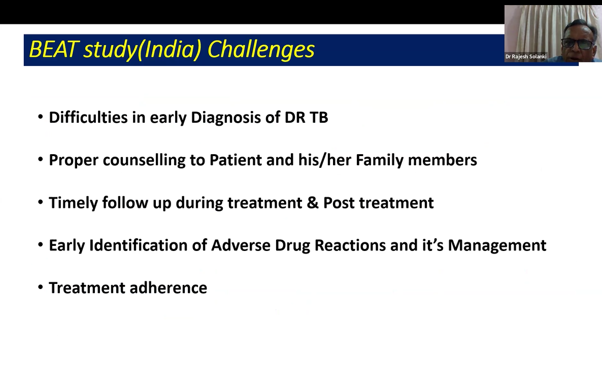
Adding a complementary perspective, Dr. Solanki Rajesh Natvarlal, principal investigator of the BEAT TB India study, shared early implementation experiences from one of the world’s most challenging DR-TB contexts. The BEAT TB India cohort included patients with low body mass index (BMI), advanced disease, and exceptionally high fluoroquinolone resistance (96%); situations where short regimens are often difficult to operationalize.
Despite these complexities, BDLC demonstrated 91% favorable outcomes among patients who completed treatment, with rapid culture conversion (75% by week 8 and 98% by week 20) and strong durability at 48 weeks. These results signal that BDLLfxC can be a viable option even in high-burden, resource-diverse settings.
What this means for TB Programs and the future of care
While evidence from South Africa and India continues to strengthen the case for BDLLfxC, the discussion also pointed toward what comes next. Countries are beginning to explore how this regimen may fit their current diagnostic capacity, patient flow, and clinical infrastructure. Questions on monitoring for linezolid-related adverse events, managing adolescents, and handling late culture conversion reflect a growing interest in operationalizing this regimen safely and effectively. The momentum around BDLLfxC also signals demand for more tailored DR-TB treatment for specific vulnerable populations.
As PeerLINC continues facilitating cross-country learning, sessions like this help programs translate evidence into practice, adapting global guidance into workable national policy and ensuring PeerLINC remains a catalyst in the global movement for equitable, flexible care and continued people-centered innovation.